Pneumococci
Pneumococci were first noticed in 1881 by Pasteur and Sternberg independently. They produce a fatal septicemia in rabbit by inoculating human saliva and isolated pneumococci from the blood of the animals. Relationship among pneumococci and pneumonia was established only later by Fraenkel and Weichselbaum independently in 1886.
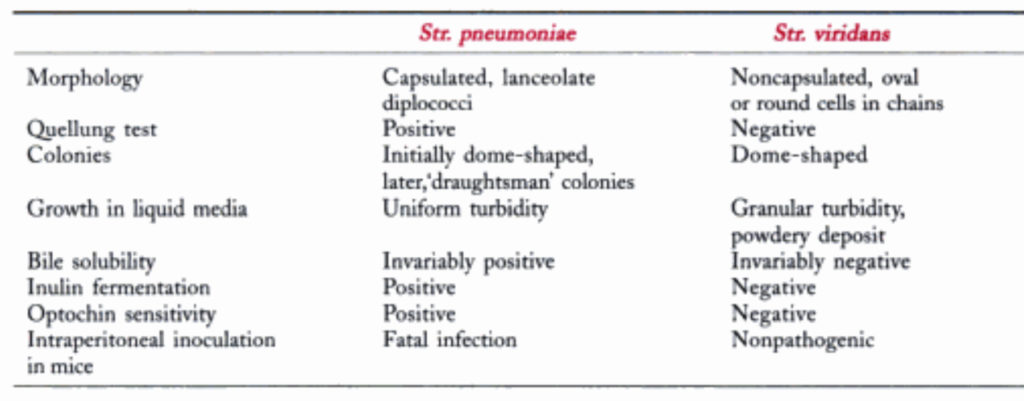
Pneumococcus is a Gram positive lanceolate diplodocus. Because of its genetic relatedness to streptococcus, it is classified as str. pneumonia.
Pneumococcus differs from other streptococci chiefly in its morphology, bile solubility, optochin sensitivity and possession of a specific polysaccharide capsule.
Pneumococci are normal inhabitants of the human upper respiratory tract. They are the single most prevalent bacterial agent in pneumonia and in otitis media in children.
Pneumococci can also cause sinusitis, bronchitis, infections bacteremia, meningitis and other infections.
Morphology
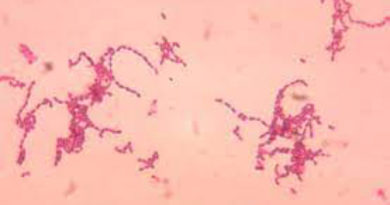
Pneumococci are typically small (1 micrometer), slightly elongated cocci, with one end broad or rounded and the other pointed, presenting a flame shaped or lanceolate appearance.
They occur in pairs (diplodocui), with the broad ends in apposition, the long axis of the coccus parallel to the line joining the two cocci in a pair. They are capsulated, the capsule enclosing each pair.
In culture, the typical morphology may not be apparent and the cocci are more rounded, tending to occur in short chains. They are nonmotile and non sporing. The capsule may be demonstrated as a clear halo in Indian ink preparations or may be stained directly by special techniques.
Cultural Characteristics
Pneumococci have complex growth requirements and grow only in enriched media. They are aerobes and facultative anaerobes, the optimum temperature being 37 C (range 25 – 42 C) and pH 7.8 (range 6.5 – 8.3). growth is improved by 5 – 10% CO2.
On blood agar, after incubation for 18 hours, the colonies are small (0.5 – 1 mm), dome shaped and blistering, with an area of green discoloration (alpha hemolysis) around them, resembling colonies of Str. vairidans. On further incubation the colonies become flat with raised edges and central umbonation.
Under anaerobic conditions, colonies on blood agar are surrounded by a zone of beta hemolysis due to oxygen labile hemolysis O.
In liquid media such as glucose broth, growth occurs as uniform turbidity.
Biochemical Reactions
Pneumococci ferment several sugars, forming acid only. Fermentation of insulin by pneumococci is a useful test for differentiating them from streptococci as the latter do not ferment it.
Pneumococci are bile soluble. If a few drops of 10% sodium deoxycholare solution are added to 1 ml of an overnight broth culture, the culture clears due to the lysis of the cocci.
Bile solubility is a constant property of pneumococci and hence is of diagnostic importance.
Pneumococci are catalase and oxidase negative.
Resistance
Pneumococci are delicate organisms and are readily destroyed by heat (thermal death point 52 C for 15 minutes) and antiseptics. In cultures, they die on prolonged incubation, perhaps due to an accumulation of toxic peroxides.
They are sensitive to most antibiotics, beta lactams being the drug of choice. Almost all strains were sensitive to 0.05 mg penicillin till 1967, when the resistant strains began to appear.
A drug resistant Strep. Pneumonia (DRSP) strain originating in spain has spread to most parts of the world posing problems in treatment.
Variation
On repeated subculture, pneumococci undergo a smooth to rough (S – R) variation. In the R form, the colonies are rough and the cocci are non capsulated, autoagglutinable and avirulent. R forms arise as spontaneous mutates and outgrow the parental S forms in artificial culture; in tissues, such R mutants are eliminated by phagocytosis.
Toxins And Other Virulence Factors
Pneumococci produce an oxygen labile hemolysis and a leucocidin but these are weak and make no contribution to virulence. The virulence of pneumococci depends on its capsule and the production of a toxin called pneumolysin. The capsule polysaccharide, because of its acidic and hydrophilic properties, protects the cocci from phagocytosis. They are however, susceptible to ‘surface phagocytosis’, being engulfed against a firm surface, such as fibrin clot or epithelium.
Pathogenicity
Experimentally, fatal infection can be produced in mice or rabbits by intraperitoneal inoculation of pneumococci. Death occurs in 1 – 3 days, and pneumococci can be demonstrated in large numbers in the peritoneal exudate and heart blood.
Pneumococci colonies the human nasopharyngeal and may cause infection of the middle ear, paranasal sinuses and respiratory tract by direct spread. Infection of the meninges can also occur, by contiguity or through blood.
Pneumococcal bacteremia may also lead to distant infection as in the heart, peritoneum or joints. Infection is commonly endogenous, but exogenous infection may also occur, especially with highly virulent strains.
Pneumococci are one of the most common bacteria causing pneumonia, both lobar and bronchopneumonia. They also cause acute trachea bronchitis and empyema.
Laboratory Diagnosis
The clinical diagnosis of pneumonia is easy but as the disease may be caused by several different microorganisms, etiological diagnosis should be made by laboratory tests. This is of great importance in treatment.
They may be demonstrated by Gram stain. The sputum, after homogenization if necessary, is inoculated on blood agar plates and incubated at 37 C under 5 – 10 % CO2. Growth occurs after overnight incubation. Where sputum is not available, as in infants, serum – coated laryngeal swabs may be used for culture. Isolation from respiratory secretions is facilitated by using blood agar containing gentamicin 5 microgram/ml.
Treatment
The antibiotic of choice is parenterally penicillin in serious cases and amoxicillin in milder ones, provided the infecting strain in penicillin sensitive.
Many penicillin resistant strains are also resistant to other antibiotics like erythromycin and tetracycline. A third generation cephalosporin is indicated in such cases. Vancomycin is to be reserved for life threatening illnesses with highly resistant strains.
Reference
Text Book Of Microbiology