Shigella – Morphology, Cultural Character, Prophylaxis, Control
Dysentery is a clinical condition of multiple etiology, characterized by the frequent passage of blood stained, mucopurulent stools. Two common type of dysentery are because of bacillary and amebic.
The causative agents of bacillary dysentery belong to the genus Shigella.
Some other bacilli, such as E. coli, Vibrio parahaemolytius and Campylobacter, can also cause dysentery.
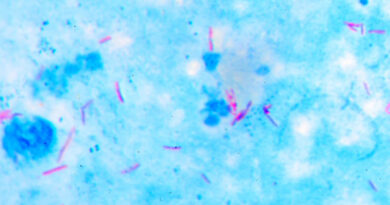
Morphology
Shigellae are Gram negative rods, they are non motile, non sporing and non capsulated. Their size range from 0.5 x 1- 3 micrometer.
Cultural Characteristics
Shigella are aerobes and facultative anaerobes, with a growth temperature range of 10 – 40 C and optima of 37 C and pH 7.4. they grow on ordinary media but less readily than other enterobacteria.
After overnight incubation, its colonies are small, about 2 mm in diameter, circular, convex, smooth and translucent. If its colonies are frequently subculture colonies may be of rough type.
Due to the absence of lactose fermentation, colonies on MacConkey agar are colorless. An exception is Sh. Sonnei which can ferment lactose late and forms pale pink colonies.
Deoxycholate citrate agar (DCA) is a useful selective medium. Growth is inhibited on Wilson and Blair’s bismuth sulphite medium.
Resistance
Shigella are not specially resistant. They are killed at 56 C in one hour and by 1% phenol in 30 minutes. In ice they last for 1 – 6 months. They remain viable in moist environments for days, but die rapidly on drying.
In feces they die within a few hours due to the acidity produced by the growth of coli form. Sh. Sonnei is in general more resistant than any other shigella species.
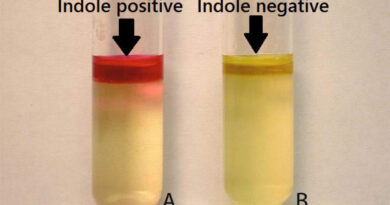
Biochemical Reactions
Shigella are MR positive and reduce nitrates to nitrites. They cannot utilize citrate as the sole source of carbon. It do not form H2S and inhibited by KCN. Catalase is produced, except by Sh. Dysenteriae type 1.
Glucose is fermented with the production of acid, without gas, except for the Newcastle and Manchester bio types of Sh. Flexneri type 6, and some strains of Sh. Boydii type 13 and 14, which form gas.
Fermentation of mannitol is of importance in classification. Shigella is traditionally divided into two categories mannitol fermenting and non fermenting.
Classification
Shigellae are classified into four species or subgroups based on a combination of biochemical and serological characteristics. Serotypes are distinguished within the species. Sh. Sonnei is serologically homogeneous and is classified by coli in typing.
Pathogenicity
Shigellae causes bacillary dysentery. Infection occurs by ingestion. The minimum infection does is low, as few as 10 – 100 bacilli being capable of initiation the disease, probably because they survive gastric acidity better than other enterobacteria.
Their pathogenic mechanisms resemble those of enteroinvasive E. coli. The bacilli infect the epithelial cells of the villi in the large intestine and multiply inside them.
Exotoxins are also produced in some species like Sh. Dysenteriaer type 1. But it appears to be much less important in pathogenesis than the ability of the bacillus to penetrate and multiply in colonic mucosa.
Bacillary dysentery has a short incubation period (1 – 7 days, usually 48 h). the onset and clinical course are variable and are largely determined by the virulence of the infecting strain. The main clinical features are frequently passage of loose, scanty feces containing blood and mucus, along with abdominal cramps and tenesmus. Fever and vomiting may be present.
Complications are most often seen in infection with Sh. dysenteriae type 1 and include arthritis, toxic neuritis, conjunctivitis, parotitis and, in children, intussusception. Hemolytic uremic syndrome may also occur as a complication in severe cases.
The severity of the disease may vary from acute fulmination dysentery to mild diarrhea. As the term bacillary dysentery refers only to the more severe causes, the term ‘shigellosis’ has been employed to include the whole spectrum of disease caused by shigellae.
Human beings are the only natural hosts for shigellae.
Laboratory diagnosis
Diagnosis is made by isolating the bacillus from feces. Fresh feces should be inoculated without delay or transported in a suitable medium such as Sachs’ buffered glycerol saline, pH 7.0 – 7.4. highly alkaline transport media used for vibrios are inhibitory for shigellae. Rectal swabs are not satisfactory.
Treatment
Uncomplicated shigellosis is a self limited condition in which the patient usually recovers spontaneously in a few days.
However, in acute cases, particularly in infants and young children, dehydration has to be corrected promptly. Oral rehydration is adequate in most cases.
Indiscriminate antibiotic treatment will only worsen the problem of drug resistance in intestinal bacteria. Antibiotics should therefore be limited to severe or toxic cases.
Control
Control consists essentially in improving personal and environmental sanitation. Antibiotics have no place in prophylaxis. No effective vaccine is available.
Reference: The Text Book Of Microbiology